
Introduction to Wilderness Medicine
In the wilderness you will have limited resources, and limited capabilities for major medical intervention. So it is important to have a basic understanding of wilderness medicine and first aid, as it could save a life. So with my medical background in trauma surgery, and the emergency room - here is an introduction to Wilderness Medicine.
Disclaimer: Please keep in mind this is a guide and you should receive additional training in order to feel confidant and comfortable in each scenario.
Initial Assessment:
The best thing to do is approach the patient using the Acronym: ABCDE, which stands for Airway, Breathing, Circulation, Disability, Exposure. The initial question before all else, is "Am I putting myself at risk by trying to save this person?". Make sure there won't be two injured people on the ground before you commit to completing the ABCDE steps. Please make sure that the scene is safe for you approach - don't approach a bleeding person with a Grizzly Bear standing over them.
Make sure to wear gloves, put on your sunglasses because you may not know them- and don't know your friends as well as you do.
For those with minimal medical knowledge, here are some questions you should ask after taking a big breath, and introducing yourself in a calm way to the injured person or suspected injured person.

Airway in Wilderness Medicine
Remove dirt or objects that you can see. Do not do blind sweeps with your fingers as this can lodge things further down the throat. They can have dirt, teeth, severed tounge etc... it might be bloody so be prepared (thus the gloves and sunglasses).
Jaw thrust - go to the head of the patient, grab their jaw (right at the angled portion) and lift it slightly forward. Do not move the neck, or tilt the head back significantly when you are doing this because they may have a major neck injury.
- In the Emergency Room they often use an nasopharyngeal tube to keep an airway open in an emergency. You can use a camel back to cut this down measuring from ear to mouth.
- Here is a video on how to properly insert a nasopharyngeal tube into a patient.
- If you don't have a nasopharyngeal tube, then you can take your knife - cut the tube on a camel back and insert that into the nose down to the airway. Be sure to measure it properly. Using the ear to jaw measurement method.
- If the camel back doesn't work, you can also use TWO safety pins pinned on either side of the tongue with a shoelace threaded through them tied to the belt loop, their finger etc... I like to have four safety pins so that the paracord/string/shoelace remains in place.
- If this wakes the patient up, then you have solved the issue of their airway, because an awake patient, can control their tongue muscles. Also, keep in mind it will feel weird grabbing a limp tounge, it might be weird and gross but it is better than that person being dead because you couldn't leave their airway while trying to treat the bleeding broken leg that may also kill them.
In the Emergency Room they often use an nasopharyngeal tube to keep an airway open in an emergency. You can use a camel back to cut this down measuring from ear to mouth.
- Here is a video on how to properly insert a nasopharyngeal tube into a patient.
Here is a video on how to properly insert a nasopharyngeal tube into a patient.
If you don't have a nasopharyngeal tube, then you can take your knife - cut the tube on a camel back and insert that into the nose down to the airway. Be sure to measure it properly. Using the ear to jaw measurement method.
If the camel back doesn't work, you can also use TWO safety pins pinned on either side of the tongue with a shoelace threaded through them tied to the belt loop, their finger etc... I like to have four safety pins so that the paracord/string/shoelace remains in place.
- If this wakes the patient up, then you have solved the issue of their airway, because an awake patient, can control their tongue muscles. Also, keep in mind it will feel weird grabbing a limp tounge, it might be weird and gross but it is better than that person being dead because you couldn't leave their airway while trying to treat the bleeding broken leg that may also kill them.
If this wakes the patient up, then you have solved the issue of their airway, because an awake patient, can control their tongue muscles. Also, keep in mind it will feel weird grabbing a limp tounge, it might be weird and gross but it is better than that person being dead because you couldn't leave their airway while trying to treat the bleeding broken leg that may also kill them.
Chin lift - you only want to do this if you are absolutely SURE that the patient has had NO head trauma.

Have they choked on something? Is there something blocking the airway?
Cricothyrotomy (The Emergency Airway): You can slit the skin right below the Adams apple and stick the knife in. You will pop (it will literally be a pop) through a couple of layers and will hear a rush of air. If you don't feel a rush of air, then you aren't in the right space. Don't dig around, in a normal weight and build individual, it should only be about a 1/2 inch below the layer of skin/fat. In larger individuals you may have to go a little deeper. You can measure a stick a straw, a camel back tube or ball point pens to the side of the neck and it will give you a good idea of how deep the tube needs to go in order to get into the airway.
- I like to keep a 14G IV Catheter with me so that I can use that to puncture into the airway. It will be large enough to help air escape, and guide you for making a larger incision in the event that you need to ventilate.
- Keep in mind that once you put an incision in this position, medical personell will not be able to insert a viable airway tube through the mouth. So only resort to this option if the upper airway is completely blocked and the patient is deteriorating.
I like to keep a 14G IV Catheter with me so that I can use that to puncture into the airway. It will be large enough to help air escape, and guide you for making a larger incision in the event that you need to ventilate.
Keep in mind that once you put an incision in this position, medical personell will not be able to insert a viable airway tube through the mouth. So only resort to this option if the upper airway is completely blocked and the patient is deteriorating.
Breathing
Do you lay them on their back or on their side? Are you sure they are breathing? What do the breaths sound like and feel like? Breathing is really important obviously, it is generally associated with death if someone isn't breathing and/or isn't breathing well. There are entire campaigns in the States to help the public become more aware about how to save a life through CPR and First Aid classes. I highly recommend going if you have the chance.
So when assessing breathing, I would review the list below before each activity or vacation. Have someone be in charge and a backup person to support them. Having someone assigned to each task, and someone assigned to be the team leader in the event of an accident will help prevent confusion.

Look for the breathing, is their chest moving?
- Is the chest moving equally? Is one rising above the other?
- Are they using nose, neck or other muscles to help them breathe?
Is the chest moving equally? Is one rising above the other?
Are they using nose, neck or other muscles to help them breathe?
Listen for their breath by putting your ear right next to their chest.
Feel the breaths by placing your hands lightly on the chest. Does it feel like broken bones grinding together or does it feel like rice krispies under their skin?
- The feeling of Rice Krispies on the chest can indicate a tension pneumothorax. This is something that cannot wait and the patient will be dead by the time someone arrives.
- Keeping a 14G IV catheter for this situation. You go very high on the chest, right below the collar bone, pick a rib high up, and stick the needle on the TOP part of the rib. (Hold onto it because the trapped air will push the needle out- if there is no rush of air, try the other side. If the rush of air is not on the other side, then take it out).
- Most of the time, people don't put the needle deep enough.
- Open Pneumothorax - this is when someone has something penetrating through their skin into their lung. This destroys the physics of the lung and how we breathe. So if there is a hole in the chest, with abnormal breathing - take a plastic baggie, take your duct tape and tape ONLY THREE Sides flat onto the chest (so that air can get OUT of one side).
- Do not EVER remove an impaled object into the chest area, or into the leg area.
The feeling of Rice Krispies on the chest can indicate a tension pneumothorax. This is something that cannot wait and the patient will be dead by the time someone arrives.
- Keeping a 14G IV catheter for this situation. You go very high on the chest, right below the collar bone, pick a rib high up, and stick the needle on the TOP part of the rib. (Hold onto it because the trapped air will push the needle out- if there is no rush of air, try the other side. If the rush of air is not on the other side, then take it out).
- Most of the time, people don't put the needle deep enough.
Keeping a 14G IV catheter for this situation. You go very high on the chest, right below the collar bone, pick a rib high up, and stick the needle on the TOP part of the rib. (Hold onto it because the trapped air will push the needle out- if there is no rush of air, try the other side. If the rush of air is not on the other side, then take it out).
Most of the time, people don't put the needle deep enough.
Open Pneumothorax - this is when someone has something penetrating through their skin into their lung. This destroys the physics of the lung and how we breathe. So if there is a hole in the chest, with abnormal breathing - take a plastic baggie, take your duct tape and tape ONLY THREE Sides flat onto the chest (so that air can get OUT of one side).
- Do not EVER remove an impaled object into the chest area, or into the leg area.
Do not EVER remove an impaled object into the chest area, or into the leg area.
Basic Life Support would suggest giving breath's (use a glove as a barrier for rescue breathing- tear off the middle finger and put your mouth in the opening to give breaths) to the patient and doing chest compressions. Contact your local hospital to get education on how to do this. In the USA the Red Cross does BLS courses in the community.
Circulation in Wilderness Medicine
First things first, if they aren't already laying down - ask them to lie down. If you know how to take a pulse (near the thumb, or on the neck on either side of the neck right near their windpipe) see what their heart rate is. A normal adult should have a heart beat from 70-80 beats per minute.

Check their skin color, are they pale, cool, moist? If you answered yes, they may have an issue with their circulation or are in shock.
If you press down on their fingernails does the blood come back into the fingernail within <2 seconds? If it doesn't, they may be losing a lot of blood, or being going into severe shock. This method is called checking capillary refill time.
If it looks like they have a lot of the symptoms described above, or you can't feel the pulse on the wrist - you may not be able to see the bleeding that the patient is experiencing. Some of this bleeding can be internal, so raising the legs (only raise the legs that are uninjured) it can be a way to increase the blood pressure and keep blood pressure up to the brain.
If there are any areas on the surface of the body make sure to hold direct pressure for 10-15 minutes. Don't let the pressure go and check to see if it is still bleeding until that 10-15 minutes is up. If you have quick clot, pour that on and hold pressure.
For Wounds/lacerations you can use crazy glue, duct tape, staples (even the small stationary staples), or the hair closure technique.
Hair Closure technique: If the hair is more than 1-2 inches long, you can take small pieces on either side of the wound, and twist them around each other tightly. Lay them down flat against the scalp, and put crazy glue on the knot on the top of the head.
If there is a lot of debri in the wound, you can use the sterile saline rinse kits they have over the counter that people use for sinus irrigation, or they also come in small disposable packs. You can also use water (with chlorine tablets dropped in) inside a bag with small holes poked in it to irrigate it out. You can use garbage bags, condoms, sandwich bags etc.. to bring enough water to clean out the wound.
- In the Operating Room we had a saying, "The Solution to Pollution is Dilution" - and oh how true that is.
- Just keep in mind, you don't want to close a wound unless it is life threatening. Just clean the wound as well as you can, and then put pressure on it. If you close it completely then they have to keep the wound open for irrigation and it closes on its own leaving a massive scar. If it is a life threatening opening that won't stop bleeding even with pressure, then there isn't a choice but to close the wound.
In the Operating Room we had a saying, "The Solution to Pollution is Dilution" - and oh how true that is.
Just keep in mind, you don't want to close a wound unless it is life threatening. Just clean the wound as well as you can, and then put pressure on it. If you close it completely then they have to keep the wound open for irrigation and it closes on its own leaving a massive scar. If it is a life threatening opening that won't stop bleeding even with pressure, then there isn't a choice but to close the wound.

If the bleeding is coming from the legs or arms, putting a tourniquet on the limb using a stick slid just underneath the knot (turning it slowly until the bleeding stops). Make some kind of mark on the patient to make sure that someone knows a tourniquet has been placed.
If a tourniquet is left on for more than 6 hours they are at risk of losing their limb. You are ok to release the tourniquet after 6 hours, as long as the bleeding from the limb is not life threatening. Leave it off for at least 20 minutes to 1 hour (as bleeding allows) then replace it.
If you don't have quick clot, you can use duct tape, crazy glue (but not for lots of bleeding as it won't stick), hair ties, staples. If someone has an epi pen for allergies- you can use that injected into the body. There are certain places they say NOT to use any kind of Epi (Fingers, Toes, Penis, Nose) - but again, if it is life threatening....then just do it).
Many medical personell don't know how to use Epi pens if you ask them, they will likely go into their office or look up how on their phones. So it is really simple...take off the caps and THE ORANGE PART GOES INTO THE PATIENT. Don't stick it in quickly and pull it out once you push the button on the top, as it takes 10 FULL seconds to get the epi (the medicine) into the patient.
Disability
Are they talking normally, confused (name, date, location, what they were doing), responding with a loud voice, do they respond to pain (pinch them on the wrists and behind the ear)? Are their pupils equal? Do the pupils respond to light (use your phone light)? Are they able to move both arms and both legs?

The reason you want to do this as the initial portion for 'D' is to see what type of transportation you need for this person. If their pupils aren't reacting like they should, if they do not respond to pain stimuli, or they are confused - then there is likely something going on with their brain and they need immediate attention via a helicopter transport that would get them the medical attention necessary to save as much of their brain as possible.
Neck Injury
Always assume they have a neck injury if they have had a head injury, major injuries or broken bones, they are intoxicated, or were hit by a moving vehicle or boat. Do not believe them when they say their neck is fine, there are plenty of times in the moment of the Adrenalin rush that they won't feel the trauma that is there.

In this case you want to imagine the patient as a log. everything should remain in line, and no turning, pulling pushing on the spine or neck.
Improvising to protect their neck - you want to prevent them from flexing their neck and turning it side to side:
- Preventing Forward Neck Flexion
- Aluminum Splints area a great way to splint not just a fracture, but you can thread these behind the neck, and then cut it down so it encircles it once.
- A really bulky sweater wrapped around the neck and duct taped on also works
- Prevent them from looking side to side with Side Rolls
- Improvise with: Water bottles duct taped to the side of the neck to keep it in place. paddles on both sides crossed over the chest, taping sticks together and wrapping a shirt around the ends to prevent punctures, putting their shoes on either side of their neck, stuff sacks or a back pack (filled with sand, clothes) put on both sides and duct tape it together.
Preventing Forward Neck Flexion
- Aluminum Splints area a great way to splint not just a fracture, but you can thread these behind the neck, and then cut it down so it encircles it once.
- A really bulky sweater wrapped around the neck and duct taped on also works
Aluminum Splints area a great way to splint not just a fracture, but you can thread these behind the neck, and then cut it down so it encircles it once.
A really bulky sweater wrapped around the neck and duct taped on also works
Prevent them from looking side to side with Side Rolls
- Improvise with: Water bottles duct taped to the side of the neck to keep it in place. paddles on both sides crossed over the chest, taping sticks together and wrapping a shirt around the ends to prevent punctures, putting their shoes on either side of their neck, stuff sacks or a back pack (filled with sand, clothes) put on both sides and duct tape it together.
Improvise with: Water bottles duct taped to the side of the neck to keep it in place. paddles on both sides crossed over the chest, taping sticks together and wrapping a shirt around the ends to prevent punctures, putting their shoes on either side of their neck, stuff sacks or a back pack (filled with sand, clothes) put on both sides and duct tape it together.

Exposure
What are the weather conditions like? Do you, or can you move them to a better location without causing pain or further damage?
For cold environments you want to try and keep them warm. Use something to block the wind.
- You can also use a garbage bag wrapped around and underneath them (as a improvised shirt or pants) with DRY leaves or other clothing stuffed inside of it to keep the heat in.
- Make sure whatever you stuff into the bag is DRY, no exceptions.
- Using a sleeping bag is also a great idea (only if not wet).
- The ground is very cold, even the dirt - so don't forget to wrap their entire body.
- It can be 85 degrees outside, and someone in shock will still be shivering relentlessly.
You can also use a garbage bag wrapped around and underneath them (as a improvised shirt or pants) with DRY leaves or other clothing stuffed inside of it to keep the heat in.
- Make sure whatever you stuff into the bag is DRY, no exceptions.
Make sure whatever you stuff into the bag is DRY, no exceptions.
Using a sleeping bag is also a great idea (only if not wet).
The ground is very cold, even the dirt - so don't forget to wrap their entire body.
- It can be 85 degrees outside, and someone in shock will still be shivering relentlessly.
It can be 85 degrees outside, and someone in shock will still be shivering relentlessly.
Were they impaled with any objects?
If there is an object that impaled the patient and is stuck in them --- DO NOT REMOVE THIS AS IT CAN CAUSE FURTHER DAMAGE!
- A good example of this, is when Steve Irwin was stung by stingray rebarbs, he quickly removed them and one was in his heart. When he removed it, it created an outlet for bleeding to happen around and from his heart causing his death.
A good example of this, is when Steve Irwin was stung by stingray rebarbs, he quickly removed them and one was in his heart. When he removed it, it created an outlet for bleeding to happen around and from his heart causing his death.
You can wrap something around the impaled object to stabilize it until the patient can get to the operating room to have it taken out. Even doctors in the Emergency Room don't typically mess with these things until you know for CERTAIN that an object has not severed an artery.
Invest in a Good First Aid Kit (not just ones with bandaids)
There are thousands of First Aid Kits out there, but how do you know which one if the best? Think of your situation, how much you are willing to put in the suitcase?
I was looking into getting an updated First Aid Kit, and ran across the company MyMedic. This company sells tourniquets, first aid kits that fit into your pocket, all the way up to a First Aid Kit that field Medics use in the war zone. The MyMedic First Aid Kit I chose, was one that specifically has quik clot in it.

This First Aid Kit has so many good things in it! I'm sincerely impressed with everything in here. It is so compact too, it is smaller than my makeup bag (and I don't wear a lot) yet has everything I would want in an emergency other than an AED and a back board. They have built the outside of the bag so you won't lose any space on your backpack with loops to hang carabiners off of.
On the back there are two button straps you could also use to hang onto your bag. You can unclip the strap that goes around the bag and use that as a neck brace with the rolled clothing or water bottles and cinch it down.
Inside it is very well organized with straps holding everything in place, just like you would find in a paramedic bag. There is benedryl, tylenol, advil, sunscreen, electrolytes, 2 pairs of gloves. Sterile bandage, triangle bandage, emergency blanket, suture kit, scissors, tweezers, sterile saline, ace wrap, tourniquet (the fancy kind), paracord, QuikClot, snap light, whistle, medical tape, bandaids, Nasopharyngeal tube, hydrogel (used for severe burns - to help slow damage to lower levels), CPR shield (so you don't have to use a glove).
This is just to name a few of the things tightly compacted into this bag. The bag also is easy to close once you are done exploring it.

Another thing I do when I go camping, hiking, climbing, or any other adventuring - I always make sure everyone knows where the first aid kit is. You put it in the same spot every time you go out adventuring. If it is on your backpack, or in your backpack, you make sure that people know how to access it. If it is in your car, make sure they know where the keys are to open the car.
If I were to add a few more things to this MyMedic Pack, I would add an Epi Pen, 14G IV Catheter, strap my swiss army knife to the outside. I would also put 4 safety pins, chlorine tablets, and crazy glue.
Just like Duct Tape, Safety Pins have so many uses, so I would highly recommend always keeping a few handy:
Tongue Extension, making eyeglasses, removing foreign bodies from skin, cornea, abscess drainage, removing a fishhook, T-shirt arm splint, sewing needle, wound closure, unclogging camping stove jet, tick removal, fix zippers/bindings, and last but not least for all my ladies out there - they work great for separating eyelashes after putting mascara on ;)
When Do You Evacuate Someone?
If the patient is having any of the following, you will likely need to ask for a helicopter or rescue team evacuation:

Breathing difficulties
Dizzy/weak/weak pulse
Unconscious/Confused
Trouble Breathing
Neck or Torso Pain
Unable to Walk
Visible Bone or Clear Dislocation
Unsure of Severity of Injury
Animal Bites and Stings in Wilderness Medicine
Know the area, animals that frequently attack - an easy way to know this is to ask a local. If you ask the concierge, the taxi driver, the ticket counter, or even your guide should know.
When I was hiking in Jamaica through the Jungle, we emerged and I felt a pinch on the skin of my foot. In the States, ticks are known to hold Lyme Disease- but my guide was able to dislodge the tick, and said that Jamaica didn't have Lyme Disease like the States did. She was from New York, and one of the toughest ladies I have ever met. So even common pests like this, may not be dangerous in the places that you visit - they may be...just pests.

This is why it is important to just ask questions about dangers when hiking in certain areas, or animals. The animal world is always changing, and animals can be quite territorial, or hide in places you may not think of.
For example, where I live, we have to keep our dogs out of the weeds in certain places we go hiking as Rattlesnakes are quite common here. You likely wouldn't find Rattlesnakes while hiking in Zermatt Switzerland. So get educated and be prepared.
Snake Bites: Move away from the snake, take off any tight clothing, do not use a tourniquet. Take a photo of the snake if possible. Call 911 to minimize having to move and increase the circulation of the poison.
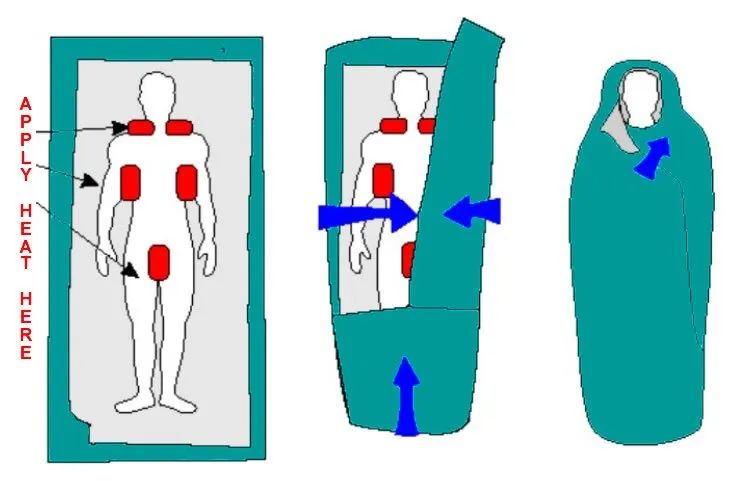
Hypothermia in Wilderness Medicine
The first time I personally experienced Hypothermia was when I went camping and hiking on Mount Whitney in November. You don't really know that you are getting cold until things start to turn blue (especially if you are exercising). Make sure to read about my whole experience there.
If you encounter someone who has Hypothermia, or if you yourself start to experience it - there are some things you can take with you. Hand warmers (the 12 hour ones are best) I would bring at least 6 for each person, or more if you are car camping. An emergency blanket, if I am backpacking or camping I will typically bring a compact Mylar blanket, and then a cloth emergency blanket over that that you can find at REI and are easy to put on your backpack.
Hyperthermia in Wilderness Medicine
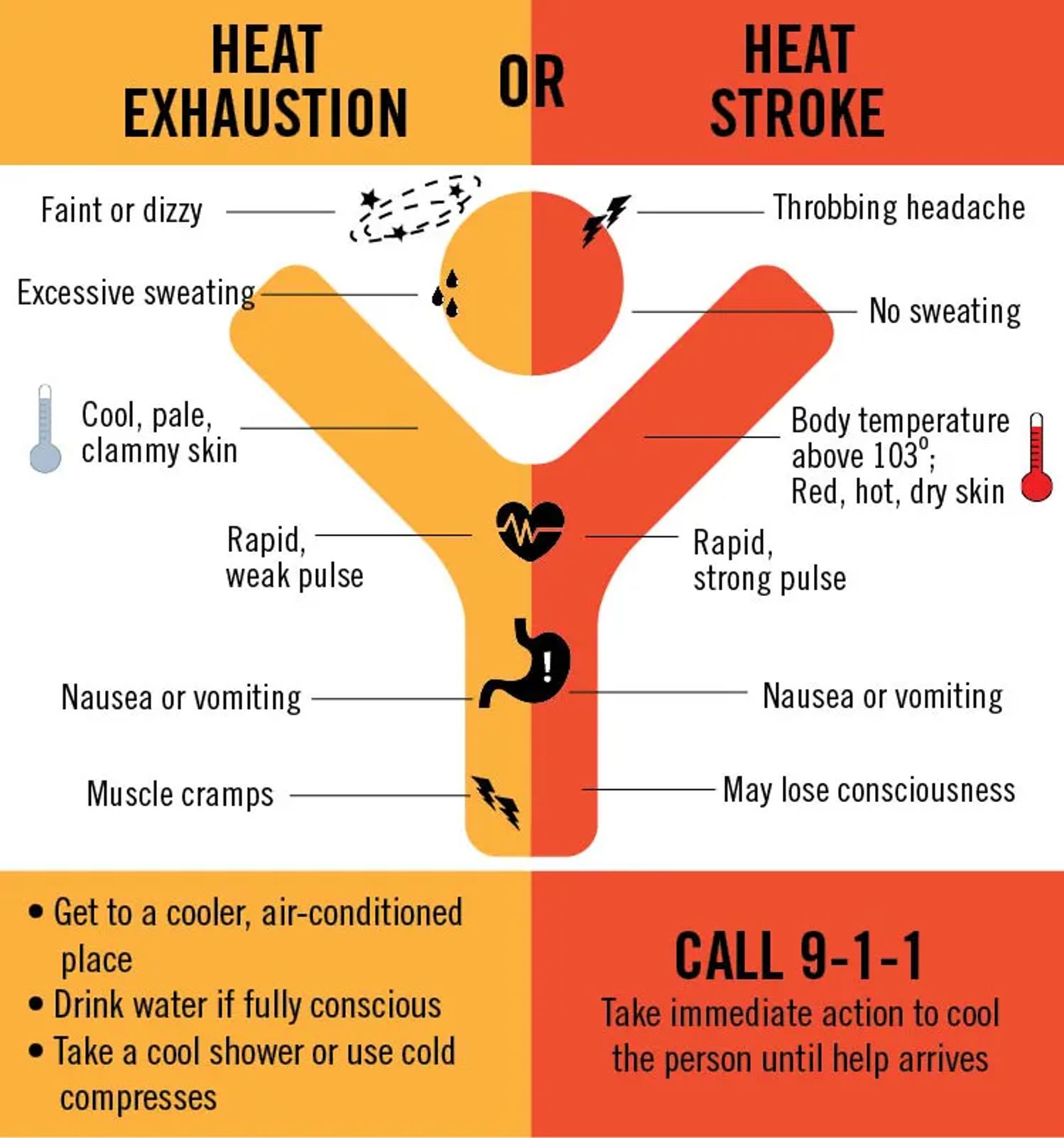
The first time I experienced Heat exhaustion was hiking in Zion National Park in the sun when it was 112 F (44C). Ever since that time I have been easily prone to heat exhaustion (another reason I sweat like a whore in church in any kind of humidity).
It starts with a dry mouth, then you get hot and start sweating so much you can hardly keep it off your body. Then it feels like your heart is going to beat out of your chest. It feels like it takes monumental effort to take even a few steps or keep your eyes open. Then your stomach starts to cramp, and you can get nauseated. When I got to the nausea and dizzy stage, that is when I knew I had heat exhaustion for sure. Be sure to read that first hand account, and keep yourself safe in warmer climates.
Getting Travel Insurance
Sometimes the first aid kit isn't enough, it can save a life in order to get to medical care though. When you are traveling abroad, you won't know what hospital is a good one, or what the cost will be. This is why I highly encourage Travel Insurance.

Not only do they help with repatriation (arrange for your body to be transported back home), they also can help with delayed or canceled flights, long term hospitalizations abroad etc..
I recommend World Nomad Insurance, because it is highly customizable. Even for coverage for my diving trip in Cabo San Lucas, for my age it was only around $69 for repatriation coverage, hospitalization, cancelled flights, delayed flights and more. For everything that they cover, I was stunned....especially since I work in the medical field and know how much headache it is to cover sports like these.
Stay Aware, and Stay Safe
There is only so much that you can prepare for on a trip. There will always be the unexpected in this life, so just prepare as much as you can - get familiar with some of these Wilderness Medicine Hacks. Some people never get hurt while they are traveling, some people are so accident prone they can regail you with stories for hours. You personally may not feel you need any of this information, but you may just possibly save someone else's life should you prepare yourself with the right information and your own first aid kit. Be safe, don't be sorry you didn't prepare. The worst thing in the world to live with is the 'What If I Would Have?'
Like it? Pin it! Sharing is Caring!








Welcome to Culture Trekking!
My name is Janiel, a medical professional, and solo adventurer. I have over 23 years of international travel experience and have a sincere passion for celebrating humanity, connecting with cultures, finding unique art and adventure. I’m an advocate for animals and sustainable travel and want to invite you to join the Culture Trekking community.






